Diagnosing heart failure with preserved ejection fraction (HFpEF)
- | By Ultromics
- Articles, Heart Failure
Heart failure with preserved ejection fraction (HFpEF) has recently been recognized as the single greatest unmet need in cardiovascular medicine, overtaking heart failure with reduced ejection fraction (HFrEF) and becoming the most common form of heart failure, with a prevalence that is increasing by 1% annually.[1] Despite this, there remains no gold standard in diagnosing HFpEF.
Diagnosing HFpEF is not as straightforward when compared to diagnosing patients with HFrEF, given that the ejection fraction is normal and, therefore, similar to that of patients with non-cardiac dyspnoea.
According to the 2022 AHA/ACC/HFSA Guideline for the Management of Heart Failure, the criteria for diagnosing HFpEF includes: a normal or near-normal left ventricular ejection fraction (LVEF ≥50%), evidence of cardiac dysfunction by echocardiography (e.g., abnormal left ventricular filling and elevated filling pressures), and elevated natriuretic peptides.[2]
The sensitivity, however, varies substantially for this approach, ranging from 25% to 80%.[3-5] In addition, patients at the early stage of the disease may be assessed as normal or indeterminant.[6]
Various parameters including clinical (patient history and physical examination), biochemical (serum BNP level), hemodynamic, and radiographic data are all utilized to reach a diagnosis, given the complexity of HFpEF.[7,8]
Scoring criteria including the H2FPEF score and HFA-PEFF scores can assist in diagnosis but are not fully validated.
This article covers how HFpEF is diagnosed according to current clinical guidelines.
History and physical
A complete physical exam should be performed on all patients with suspected heart failure, alongside a review of medical history to look for comorbidities and risk factors that are strongly linked to HFpEF.[2]
Common symptoms of HFpEF can be similar to HFrEF such as dyspnea (including dyspnea on exertion, paroxysmal nocturnal dyspnea, or orthopnea) and fatigue. If present, these symptoms typically become more severe with exertion. Physical signs of heart failure (HF) (such as elevated jugular venous pressure, pulmonary rales, and lower extremity edema) may or may not be present. [9] A history of atrial fibrillation (AF), obesity, and diabetes all increase the likelihood of HFpEF. [10] (Table 1).
Table 1. Clinical, laboratory and imaging predictors of HFpEF.[11]
Some patients with HFpEF complain of chest discomfort, which might resemble angina or have more atypical characteristics. Patients who have advanced HFpEF may present with symptoms such as resting sinus tachycardia, diaphoresis, narrow pulse pressure, and peripheral vasoconstriction. Dizziness and orthostatic intolerance suggest the possibility of cardiac amyloidosis.[12]
Several established criteria for the diagnosis of heart failure based on clinical symptoms are available. One example is the Framingham criteria, which base the diagnosis on the presence of major symptoms (such as nocturnal dyspnea and orthopnea, among others) as well as minor symptoms (such as edema of the extremities and exertional dyspnea, among others). [13]
However, Framingham's clinical criteria has excellent sensitivity to exclude the diagnosis of HF in the absence of these symptoms/signs, but it has poor specificity to confirm the diagnosis. On the other hand, some patients with HF may not have symptoms. Only 50% of patients with left ventricular (LV) dysfunction on an echocardiogram are symptomatic. Symptoms and signs of HF are either too nonspecific or too infrequent, which makes the clinical diagnosis of HF challenging with <25% of accuracy for most of the clinical features.[14]
Imaging
Echocardiography remains the main evaluation for HFpEF and provides essential information to estimate elevated LV filling pressure. The most robust indicators include Doppler transthoracic echocardiography (E/e′) to evaluate LVEF, and pulmonary artery systolic pressure (PASP), to assess left ventricular filling pressure.[11]
Other findings that increase the probability of HFpEF include left atrial enlargement, reduced left atrial strain, impaired LV early diastolic tissue velocity (e′), reduced global longitudinal strain, and right ventricular (RV) dilatation or dysfunction. (Table 1).[11]
However, echocardiography parameters are specific but have low sensitivity, and are most useful for diagnosis when abnormalities are present but do not exclude disease when absent. [15]
In patients who are clinically euvolemic, mildly hypervolemic, or early in their disease state, echocardiography-based pressure and volume criteria for diastolic dysfunction may be normal or indeterminate. Diastolic dysfunction cannot be observed by echocardiography at rest in one-third of patients with HFpEF. [15]
If cardiac filling pressures cannot be adequately assessed by echocardiography, alternative methods may be used.

Dr Patricia A. Pellikka from Mayo Clinic recently commented that HFpEF diagnosis could be simplified through echocardiography using a novel AI tool to detect HFpEF. EchoGo Heart Failure is FDA cleared and recognized as a clinical breakthrough designation. Learn more
Natriuretic peptides
Measurement of natriuretic peptides (NPs) like BNP/NT-proBNP is also helpful in supporting HFpEF diagnosis when the cause of dyspnea is unclear and the physical examination is equivocal.
Plasma natriuretic peptide levels increase in response to elevations in cardiac wall stress, which is related to chamber dimension and distending pressure according to the law of Laplace.[16] Similar to HFrEF, patients with HFpEF and elevated natriuretic peptide levels have an increased risk of HF.
Given that natriuretic peptide levels are easy to measure, they have been recommended in international guidelines. However, because one third of patients with HFpEF have normal NP levels, relying solely on their values for diagnosis is not recommended and their value must be interpreted in the clinical context. As such, the diagnostic gold standard is cardiac catheterization showing increased LV filling pressures.[16]
Exercise and invasive testing
The diagnostic conundrum in these patients has led to the introduction of invasive stress methods to evaluate HFpEF, where cardiac filling pressures are alleviated exclusively during hemodynamic exercise testing. [17-21]
This testing involves right heart catheterization for the direct measurement of central hemodynamics at rest and then during graded increases in exercise workload to volitional fatigue, ideally with simultaneous expired gas analysis to evaluate aerobic capacity (peak oxygen consumption).
A positive diagnosis of HFpEF is defined as elevated PCWP at rest (≥15 mm Hg) or during exercise (≥25 mm).[17]
Because invasive exercise testing directly assesses the parameters that define HFpEF (Table 1), this measurement serves as the gold standard test to prove (or refute) that HFpEF is the cause of symptoms.[11] However, despite it being very accurate, it is more expensive, requires operator expertise, and is not desired due to being invasive.
Exercise echocardiography has increasingly been advocated for as an alternative to invasive stress testing.[22] Some studies have shown robust correlations of variables measured using exercise echocardiography with invasively obtained data, but other studies have not reproduced these favorable results. [23]
Integrated diagnostic approaches
The clinical composite score H2FPEF[11] may also be used to aid risk stratification and to guide diagnostic workup. This score combines patient risk factors, such as obesity, AF, and age greater than 60, into a weighted score. Patients with a score of less than 2 have a low likelihood of having HFpEF, whereas patients with a score greater than 6 have a high likelihood of this disorder. A further workup is indicated for patients in the midrange of the score. (Figure 1)
This method enables a Bayesian approach to HFpEF diagnosis, whereby patients with a low or high likelihood of disease are diagnosed, and the more costly and definitive tests are reserved for patients with an intermediate pre-test probability of disease. Importantly, the H2FPEF score can be calculated using simple clinical characteristics and echocardiographic data that are universally available in clinical practice.
In 2019, a further scoring algorithm, the HFA–PEFF score, was recommended by the ESC/HFA to help guide the diagnostic evaluation of HFpEF.(Fig.1)[20] Although the recommended diagnostic algorithm is not evidence-based like the H2FPEF score, the approach is very similar.
Figure 1. Diagnostic approach for HFpEF. In the patient with unexplained dyspnoea, assessment of the pre-test probability that heart failure with preserved ejection fraction (HFpEF) is present is first performed via clinical, echocardiographic and laboratory testing. Two scoring systems have been developed for this purpose: the H2FPEF score (left) and the HFA–PEFF score (right).
Further HFpEF classification
Based on symptoms, laboratory findings, and imaging, the diagnosis of heart failure may be further classified. According to the 2022 ACCF/AHA Guidelines, heart failure may be divided into four stages based on the presence of structural changes and the presence of symptoms.[2]
-
Stage A: At risk for heart failure; patients at high risk for heart failure but no structural heart disease or symptoms of heart failure.
-
Stage B: Pre-heart failure; patients who have asymptomatic left ventricular dysfunction but no symptoms.
-
Stage C: Symptomatic heart failure; patients who have heart failure symptoms.
-
Stage D: Advanced heart failure; patients with refractory heart failure despite optimized treatment.
Additionally, heart failure is classified into New York Heart Association (NYHA) classes based on how heart failure symptoms affect the patient’s daily physical activities and functioning:
- Class I: Patients who have asymptomatic left ventricular dysfunction with no limitations on physical activity or symptoms.
- Class II: Patients who have mild symptoms with slight limitations of physical activity.
- Class III: Patients who have moderate symptoms with a marked limitation of physical activity.
- Class IV: Patients who have severe symptoms at rest. [1]
A clearer path needed for HFpEF diagnosis
As HFpEF continues to grow in scope, more sensitive tools to identify, phenotype, and track therapeutic improvement are needed.
Diagnosis relies on the demonstration of objective evidence of cardiac dysfunction, on the basis of either physical examination, imaging data, blood testing results or echocardiography data. When these tests are inconclusive, invasive exercise testing is necessary, which has its own set of limitations.
Earlier detection and more precisely identifying who actually has HFpEF is one of the most important ways to improve the quality of life and long-term prognosis for patients with HFpEF.
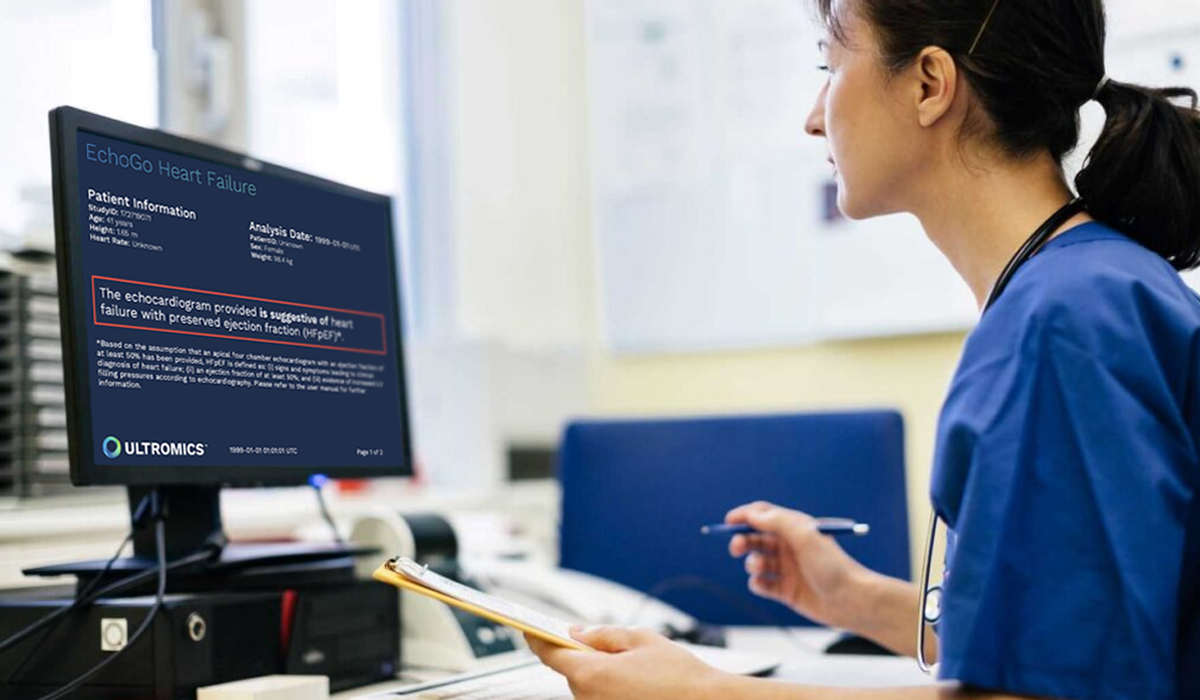
Ultromics has developed the first integrated platform, connecting echocardiography and AI, to help clinicians detect HFpEF earlier so they can determine who needs treatment — and who doesn’t. Learn about how EchoGo Heart Failure can support accurate HFpEF diagnosis.
References:
- Bryan Stringer, et al. Journal of Cardiac Failure, 2022.
- Heidenreich PA, et al. J Card Fail, 2022.
- Penicka M, Bartunek, et al. J Am Coll Cardiol. 2010.
- Lam CS, Roger VL, Rodeheffer RJ, Borlaug BA et al. J Am Coll Cardiol, 2009.
- Obokata M, Reddy YNV, Borlaug BA, et al. Heart Fail Clin. 2018.
- Mitter SS, Shah SJ, Thomas JD. et al. J Am Coll Cardiol, 2017.
- Zakeri R, Cowie MR et al. Heart, 2018.
- Huis in ’t Veld AE, de Man FS, van Rossum AC, Handoko ML et al. Neth Hear J, 2016.
- Solomon SD, Rizkala AR, Lefkowitz MP, Shi VC, Gong J, Anavekar N, et al. Circ Heart Fail, 2018.
- Milton Packer et al. Eur J Heart Fail, 2020.
- Reddy, Y. N. V., Carter, R. E., Obokata, M., Redfield, M. M. & Borlaug, et al. Circulation, 2018.
- Barry A. Borlaug et al. Nature Reviews Cardiology, 2020.
- Ulrika Löfström et al. ESC Heart Fail, 2019.
- Said Hajouli et al. StatPearls Publishing, 2022.
- Iwanaga, Y. et al. J. Am. Coll. Cardiol, 2016.
- De Keulenaer G.W., Brutsaert D.L et al. Circulation. 2011.
- Borlaug BA, Nishimura RA, Sorajja P, Lam CS, Redfield MM. Exercise hemodynamics enhance diagnosis of early heart failure with preserved ejection fraction. Circ Heart Fail. 2010;3:588–595.
- Obokata, M. et al.. Circulation, 2017.
- Reddy, Y. N. V., Carter, R. E., Obokata, M., Redfield, M. M. & Borlaug, B. A et al. Circulation, 2018.
- Pieske, B. et al. Eur. Heart J, 2019.
- Heart Failure Association (HFA) of the European Society of Cardiology (ESC). Eur. Heart J, 2019.
- Obokata, M. et al. Circulation, 2017.
- Maeder, M. T., Thompson, B. R., Brunner-La Rocca, H. P. & Kaye, D. M etal.. J. Am. Coll. Cardiol, 2010.
Curious about upcoming research and innovation?
Sign up to hear about the latest news.